Componentes básicos de los programas de rehabilitación cardiaca para personas sometidas a cirugía cardiaca: una revisión de alcance
DOI:
https://doi.org/10.33194/rper.2024.385Palabras clave:
Cirugía cardíaca, Rehabilitación, Calidad de vida, Terapia de ejercicioResumen
Introducción: En la actualidad, el número de cirugías cardíacas ha aumentado, siendo una opción de final de línea cuando el tratamiento médico no logra responder a los problemas de los individuos, con el objetivo de reparar la disfunción del funcionamiento mecánico del corazón. La rehabilitación cardiaca (RC) es una intervención multidimensional que incluye la educación y la modificación de los factores de riesgo cardiovascular con el fin de mejorar la calidad de vida de las personas. Como componente central de los programas de RC, el ejercicio físico es una estrategia que promueve la mejora del rendimiento físico, así como la reducción de los síntomas asociados a la enfermedad y a la cirugía. Por estas razones, dadas las implicaciones derivadas de los procesos patológicos y quirúrgicos en los pacientes sometidos a cirugía cardíaca, es necesario definir, implementar y evaluar intervenciones que permitan minimizar el impacto funcional en los individuos afectados por estas condiciones.
Propósito: Mapear y analizar programas de RC en fase II que incluyan individuos sometidos a cirugía cardíaca clásica, con especial atención a los componentes de ejercicio físico.
Metodología: Scoping Review (ScR) basada en los principios defendidos por el Joanna Briggs Institute®. Dos revisores independientes analizaron la pertinencia de los artículos y extrajeron y sintetizaron los datos. Los criterios de elegibilidad se definieron como estudios de cualquier nivel de evidencia, que describían claramente la intervención realizada en la fase II de la RC y cuya población diana incluía individuos sometidos a bypass aortocoronario y cirugía valvular cardiaca. Se realizó una búsqueda ilimitada en las fuentes de datos EBSCOHost, Web of Science, Scopus y literatura gris.
Resultados: Se incluyeron 28 publicaciones en esta revisión. La intervención varía entre 3 semanas y 12 meses, con sesiones diarias de entrenamiento 2-5 veces por semana, de entre 30 y 60 minutos de duración. La intensidad y el tipo de ejercicio prescrito fueron áreas con una amplia dispersión, favoreciendo la mayoría de los estudios el entrenamiento anaeróbico, de intensidad baja a moderada.
Discusión: La mayoría de los programas se evalúan al inicio, a la mitad y al final del programa, utilizando escalas para medir la calidad de vida, la capacidad cardiorrespiratoria y la funcionalidad. Las características de la intervención, la duración y los instrumentos de evaluación difieren entre los estudios.
Conclusión: Deberían realizarse más investigaciones para conocer el abanico de criterios de frecuencia, intensidad, tipo y duración del ejercicio físico a implementar en personas sometidas a cirugía cardíaca en fase II de RC. La cartografía de las intervenciones que podrían utilizarse en los programas de RC de fase II podría ayudar a determinar los principales componentes que deben tenerse en cuenta en los programas de intervención, para una toma de decisiones informada por parte de la enfermería de rehabilitación, así como a identificar las áreas prioritarias de investigación.
Descargas
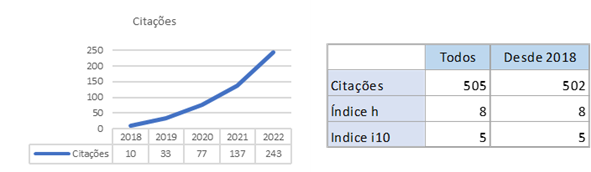
Citas
Direção Geral de Saúde. Programa Nacional Para as Doenças Cardiovasculares 2017. DGS [Internet]. 2017.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. European heart journal. 2021;42(36):3599-726.
Lai FY, Abbasciano RG, Tabberer B, Kumar T, Murphy GJ. Identifying research priorities in cardiac surgery: A report from the James Lind Alliance Priority Setting Partnership in adult heart surgery. BMJ Open. 2020;10(9).
Altinbas Y, Yavuz van Giersbergen M. Experiences of patients who had undergone coronary artery bypass graft surgery with strengths-based nursing care. Marmara Medical Journal. 2021;34(1):57-65.
Højskov IE, Moons P, Egerod I, Olsen PS, Thygesen LC, Hansen NV, et al. Early physical and psycho-educational rehabilitation in patients with coronary artery bypass grafting: A randomized controlled trial. J Rehabil Med. 2019;51(2):136-43.
Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115(20):2675-82.
Singh NV, Kalia R, Singh A, Ghai S, Shyam TS. A Methodological study to develop a cardiac rehabilitation program protocol for patients undergoing cardiac surgeries. Nursing & Midwifery Research Journal. 2021;17(4):181-90.
American College of Sports and Medicine. Guidelines for Exercise Testing and Prescription. 11 ed. Philadelphia 2021.
Laustsen S, Oestergaard LG, van Tulder M, Hjortdal VE, Petersen AK. Telemonitored exercise-based cardiac rehabilitation improves physical capacity and health-related quality of life. Journal of Telemedicine and Telecare. 2018;26(1-2):36-44.
Niebauer J. Cardiac Rehabilitation Manual 2ed. Austria 2017.
Pacaric S, Turk T, Eric I, Orkic Z, Eric AP, Milostic-Srb A, et al. Assessment of the Quality of Life in Patients before and after Coronary Artery Bypass Grafting (CABG): A Prospective Study. INTERNATIONAL JOURNAL OF ENVIRONMENTAL RESEARCH AND PUBLIC HEALTH. 2020;17(4).
Arksey H, O'Malley L. Scoping studies: towards a methodological framework. 2005.
Peters M, Godfrey C, McInerney, Parker HK, Baldini D, Soares C. Scoping reviews 2020.
Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil H. Scoping Reviews. 2020. In: JBI Manual for Evidence Synthesis [Internet]. JBI. Available from: https://synthesismanual.jbi.global. .
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467-73.
Ma C, Wang B, Zhao X, Fu F, Zheng L, Li G, et al. WeChat-based education and rehabilitation program in unprotected left main coronary artery disease patients after coronary artery bypass grafting: an effective approach in reducing anxiety, depression, loss to follow-up, and improving quality of life. Brazilian journal of medical and biological research = Revista brasileira de pesquisas medicas e biologicas. 2021;54(4):e10370.
Rakhshan M, Toufigh A, Dehghani A, Yaktatalab S. Effect of Cardiac Rehabilitation on Sexual Satisfaction Among Patients After Coronary Artery Bypass Graft Surgery. JOURNAL OF CARDIOPULMONARY REHABILITATION AND PREVENTION. 2019;39(6):E26-E30.
Pakrad F, Ahmadi F, Grace SL, Oshvandi K, Kazemnejad A. Traditional vs Extended Hybrid Cardiac Rehabilitation Based on the Continuous Care Model for Patients Who Have Undergone Coronary Artery Bypass Surgery in a Middle-Income Country: A Randomized Controlled Trial. Archives of Physical Medicine & Rehabilitation. 2021;102(11):2091-.
Moreira JMA, Grilo EN. Quality of life after coronary artery bypass graft surgery - results of cardiac rehabilitation programme. Journal of Exercise Rehabilitation. 2019;15(5):715-22.
Kraal JJ, Peek N, van den Akker-Van Marle ME, Kemps HM. Effects and costs of home-based training with telemonitoring guidance in low to moderate risk patients entering cardiac rehabilitation: The FIT@Home study. BMC Cardiovasc Disord. 2013;13:82.
Jolly K, Taylor R, Lip GY, Greenfield S, Raftery J, Mant J, et al. The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence. Health Technol Assess. 2007;11(35):1-118.
Macken LC, Yates BC, Meza J, Norman J, Barnason S, Pozehl B. Health-related quality-of-life outcomes in coronary artery bypass surgery patients and partners. J Cardiopulm Rehabil Prev. 2014;34(2):130-7.
Carlsson R. Serum cholesterol, lifestyle, working capacity and quality of life in patients with coronary artery disease. Experiences from a hospital-based secondary prevention programme. Scand Cardiovasc J Suppl. 1998;50:1-20.
Firouzabadi MG, Sherafat A, Vafaeenasab M. Effect of physical activity on the life quality of coronary artery bypass graft patients. J Med Life. 2014;7(2):260-3.
Pengelly J, Pengelly M, Lin K-Y, Royse C, Royse A, Bryant A, et al. Resistance Training Following Median Sternotomy: A Systematic Review and Meta-Analysis. Heart, lung & circulation. 2019;28(10):1549-59.
Coke LA, Staffileno BA, Braun LT, Gulanick M. Upper-body progressive resistance training improves strength and household physical activity performance in women attending cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2008;28(4):238-45; quiz 46-7.
Busch JC, Lillou D, Wittig G, Bartsch P, Willemsen D, Oldridge N, et al. Resistance and balance training improves functional capacity in very old participants attending cardiac rehabilitation after coronary bypass surgery. J Am Geriatr Soc. 2012;60(12):2270-6.
Ghroubi S, Elleuch W, Abid L, Abdenadher M, Kammoun S, Elleuch MH. Effects of a low-intensity dynamic-resistance training protocol using an isokinetic dynamometer on muscular strength and aerobic capacity after coronary artery bypass grafting. Annals of Physical and Rehabilitation Medicine. 2013;56(2):85-101.
Macchi C, Fattirolli F, Lova RM, Conti AA, Luisi ML, Intini R, et al. Early and late rehabilitation and physical training in elderly patients after cardiac surgery. Am J Phys Med Rehabil. 2007;86(10):826-34.
Jelinek HF, Huang ZQ, Khandoker AH, Chang D, Kiat H. Cardiac rehabilitation outcomes following a 6-week program of PCI and CABG Patients. Front Physiol. 2013;4:302.
Turner SC, Bethell HJ, Evans JA, Goddard JR, Mullee MA. Patient characteristics and outcomes of cardiac rehabilitation. J Cardiopulm Rehabil. 2002;22(4):253-60.
Vestfold Heartcare Study Group. Influence on lifestyle measures and five-year coronary risk by a comprehensive lifestyle intervention programme in patients with coronary heart disease. Eur J Cardiovasc Prev Rehabil. 2003;10(6):429-37.
Zhang L, Zhang L, Wang J, Ding F, Zhang S. Community health service center-based cardiac rehabilitation in patients with coronary heart disease: a prospective study. BMC Health Services Research. 2017;17(1):128.
Smith KM, Arthur HM, McKelvie RS, Kodis J. Differences in sustainability of exercise and health-related quality of life outcomes following home or hospital-based cardiac rehabilitation. Eur J Cardiovasc Prev Rehabil. 2004;11(4):313-9.
Lima AP, Nascimento IO, Oliveira ACA, Martins THS, Pereira DAG, Britto RR. Home-Based Cardiac Rehabilitation in Brazil's Public Health Care: Protocol for a Randomized Controlled Trial. JMIR Res Protoc. 2019;8(11):e13901.
Moholdt TT, Amundsen BH, Rustad LA, Wahba A, Løvø KT, Gullikstad LR, et al. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: a randomized study of cardiovascular effects and quality of life. Am Heart J. 2009;158(6):1031-7.
Oerkild B, Frederiksen M, Hansen JF, Prescott E. Home-based cardiac rehabilitation is an attractive alternative to no cardiac rehabilitation for elderly patients with coronary heart disease: results from a randomised clinical trial. BMJ Open. 2012;2(6).
Scalvini S, Zanelli E, Comini L, Tomba MD, Troise G, Giordano A. Home-based exercise rehabilitation with telemedicine following cardiac surgery. Journal of Telemedicine and Telecare. 2009;15(6):297-301.
Dos Santos TD, Pereira SN, Portela LOC, Cardoso DM, Lago PD, Dos Santos Guarda N, et al. Moderate-to-high intensity inspiratory muscle training improves the effects of combined training on exercise capacity in patients after coronary artery bypass graft surgery: A randomized clinical trial. Int J Cardiol. 2019;279:40-6.
Chludilová V, Mífková L, Pochmonova J, Várnay F, Pohanka M, Al-Mahmodi NAI, et al. Functional capacity in men after coronary artery bypass surgery influenced by physical training. Scripta Medica. 2007;80(5):203-10.
Kardis P, Sherman M, Barnett SD. Association of age and quality of life following phase II cardiac rehabilitation. J Nurs Care Qual. 2007;22(3):255-9.
Pengelly JMS, Royse AG, Bryant AL, Williams GP, Tivendale LJ, Dettmann TJ, et al. Effects of Supervised Early Resistance Training versus standard care on cognitive recovery following cardiac surgery via median sternotomy (the SEcReT study): protocol for a randomised controlled pilot study. Trials. 2020;21(1):1-14.
Ogawa H, Nakajima T, Shibasaki I, Nasuno T, Kaneda H, Katayanagi S, et al. Low-Intensity Resistance Training with Moderate Blood Flow Restriction Appears Safe and Increases Skeletal Muscle Strength and Size in Cardiovascular Surgery Patients: A Pilot Study. Journal of Clinical Medicine. 2021;10(3):547.
Abraham LN, Sibilitz KL, Berg SK, Tang LH, Risom SS, Lindschou J, et al. Exercise‐based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database of Systematic Reviews. 2021;2021(5).
Thomas RJ, Beatty AL, Beckie TM, Brewer LC, Brown TM, Forman DE, et al. Home-Based Cardiac Rehabilitation: A Scientific Statement From the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Am Coll Cardiol. 2019;74(1):133-53.
Scalvini S, Zanelli E, Comini L, Dalla Tomba M, Troise G, Febo O, et al. Home-based versus in-hospital cardiac rehabilitation after cardiac surgery: a nonrandomized controlled study. Phys Ther. 2013;93(8):1073-83.
Pengelly J, Pengelly M, Lin KY, Royse C, Karri R, Royse A, et al. Exercise Parameters and Outcome Measures Used in Cardiac Rehabilitation Programs Following Median Sternotomy in the Elderly: A Systematic Review and Meta-Analysis. Heart Lung Circ. 2019;28(10):1560-70.
Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. European heart journal. 2021;42(1):17-96.
Price KJ, Gordon BA, Bird SR, Benson AC. A review of guidelines for cardiac rehabilitation exercise programmes: Is there an international consensus? European journal of preventive cardiology. 2016;23(16):1715-33.
Hansen TB, Berg SK, Sibilitz KL, Zwisler AD, Norekvål TM, Lee A, et al. Patient perceptions of experience with cardiac rehabilitation after isolated heart valve surgery. Eur J Cardiovasc Nurs. 2018;17(1):45-53.
Rathore S, Kumar B, Tehrani S, Khanra D, Duggal B, Chandra Pant D. Cardiac rehabilitation: Appraisal of current evidence and utility of technology aided home-based cardiac rehabilitation. Indian Heart Journal. 2020;72(6):491-9.
Pio CSD, Chaves GSS, Davies P, Taylor RS, Grace SL. Interventions to promote patient utilisation of cardiac rehabilitation. COCHRANE DATABASE OF SYSTEMATIC REVIEWS. 2019(2)
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2024 Revista Portuguesa de Enfermería de Rehabilitación

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.